Infertility
Definition
A couple's inability to achieve pregnancy after one year of unprotected intercourse.
Prmary Infertility : refers to a couple who has never had a child
Secondary Infertility : at least one conception has occurred, but currently the couple cannot achieve a pregnancy.
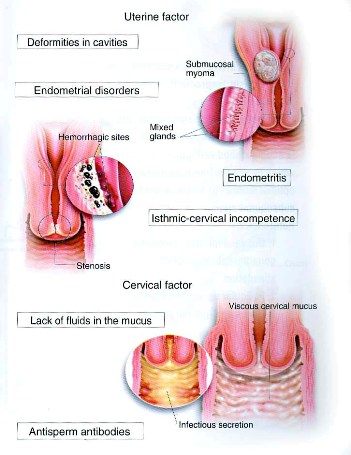
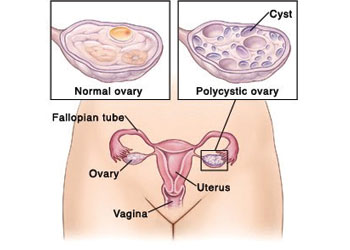
Women's Infertility
Related to
Anovulation
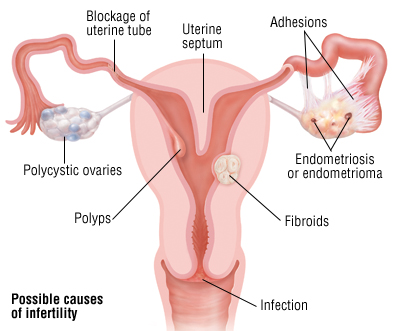
Uterine or cervical factors
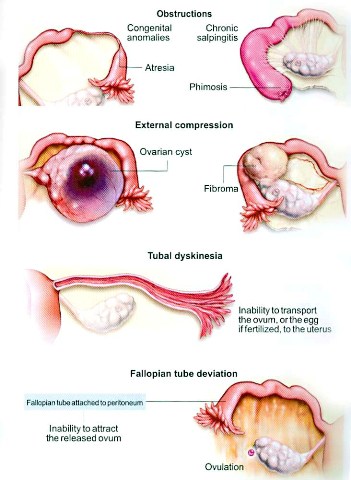
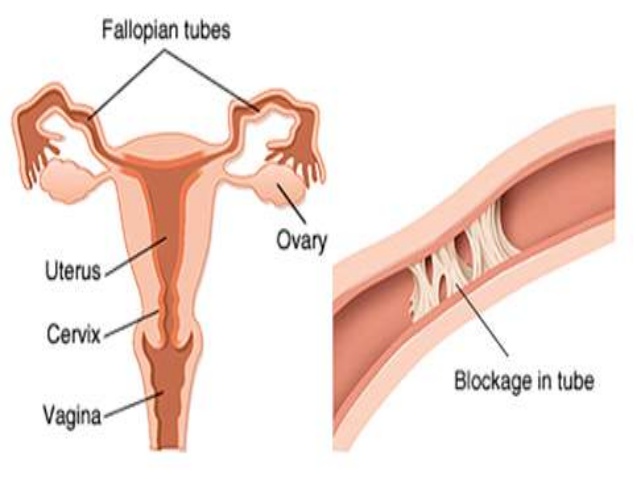
Blocked fallopian tubes
Endometriosis
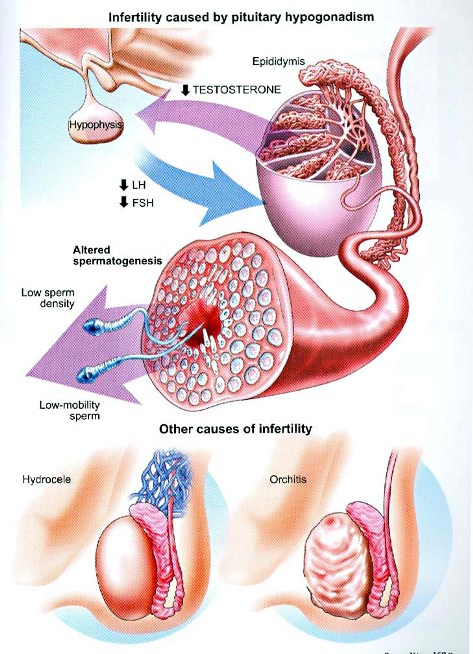
Men's Infertility
Related to
Sperm quality
Sperm production
Causes of Male Infertility
Poor lifestyle
Sexual habits out of control
Improper, irregular and unhealthy diet
Operated or damaged testicles
Alcohol, cigarette, tobacco and other toxic products
Lack of enough physical exercise
lack of enough water in body
Being on medications for very long time
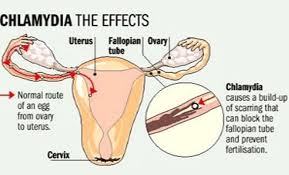
Abnormal sperm production or function due to undescended testicles, genetic defects, health problems such as diabetes, or infections such as chlamydia, gonorrhea, mumps or HIV.
Enlarged veins in the testes (varicocele) affect the quality of sperm.
Problems with the delivery of sperm due to sexual problems, such as premature ejaculation; certain genetic diseases, such as cystic fibrosis; structural problems, such as a blockage in the testicle; or damage or injury to the reproductive organs.
Overexposure to certain environmental factors, such as pesticides and other chemicals, and radiation. Cigarette smoking, alcohol, marijuana, anabolic steroids, and taking medications to treat bacterial infections, high blood pressure and depression also can affect fertility. Frequent exposure to heat, such as in saunas or hot tubs, can raise body temperature and may affect sperm production.
Damage related to cancer and its treatment, including radiation or chemotherapy. Treatment for cancer can impair sperm production, sometimes severely.
Pathophysiology
Possible causes are
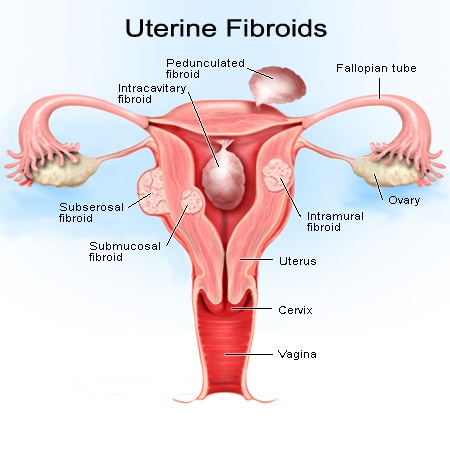
Uterine displacement by tumors, congenital anomalies and inflammation
For an ovum to be fertilized the vagina, fallopian tubes, cervix and uterus must be patent and the mucosal secretions of the cervix must be receptive to sperm. Semen and cervical secretions are alkaline, whereas normal vaginal secretions are acidic. Often more than one factor is responsible for the problem.
Assessment and diagnostic findings
Careful evaluation includes
Physical examination
Endocrinologic investigation
Consideration of psychosocial factors
Three complete histories (one of each partner and one of the couple)
Physical examination and laboratory studies are performed on both partners to rule out such causative factors as previous STDs, anomalies , injuries, tuberculosis, mumps orchitis, impaired sperm production, endometriosis, DES exposure, or antisperm antibodies.
Five factors are basic :
Ovarian: regularity of ovulation, adequacy of progestational endometrium, basal body temperature, endometrial biopsy, serum progesterone level, ovulation index
Tubal: Hysterosalpingography, Laparoscopic examination of the tubes and other pelvic structures, endometriosis
Cervical: The cervical mucus examined at ovulation and after intercourse (2to 8 hours later) to determine whether proper changes occur.
Uterine: Look for fibroids, polyps and congenital malformations by pelvic examination, hysteroscopy, saline sonogram, and hysterosalpingography.
Semen Analysis: collected after 2 to 3 days of sexual abstinence. Examined within 1 hour
Normal features of semen :
more than 1 ml
> 20 million / ml
> 50% motility
> 60% normal morphology
No sperm clumping, significant red or white blood cells, or thickening of seminal fluid (hyperviscosity)
Look for varicocele, retrograde ejaculation into the bladder
Measure testosterone, FSH, LH, prolactin levels and antisperm antibodies in blood
Medical Management
Assisted reproductive technology
Surgery to correct a malfunction or anomaly
Hormonal supplements
Proper timing
Correcting psychological or emotional factors
Pharmacologic Therapy
Clomiphene - to induce ovulation
Pulsatile gonadotropinreleasing hormone (GnRH) through infusion pump (to be worn by the woman for 1 days)
Human menopausal gonadotropin
Artificial Insemination
Sperm from partner or donor deposited into the female genital tract
Indications: Man's inability to deposit semen in the vagina due to premature ejaculation, pronounced hypospadias, dyspareunia
Abnormal cervical discharge.
A single woman's desire to have a child.
Best time selected by USGM (Ovulation)
3 - 6 inseminations over to 4 months
Usually insemination is attempted between days 10 and 1 of the cycle. Three different attempts may be made during one cycle.
All legal formalities to be followed when a donor's sperm is used and STD, HIV ruled out
In Vitro Fertilization
Ovarian stimulation
Egg retrieval
Fertilization in a test tube
Embryo transfer
Gamete intrafallopian transfer (GIFT) is a variation of IVF
Zygot intrafallopian transfer (ZIFT) may be used.
Intracytoplasmic sperm injection (ICSI) : ovum retrieved and a single sperm is injected into it and the fertilized egg is transferred to the woman. This is the method of choice in severe male factor infertility.
Nursing Management
Assist in reducing stress in the relationship
Encourage co-operation
Protect privacy
Foster understanding
Smoking is strongly discouraged
Teach about diet, exercise, stress reduction techniques, health maintenance and disease prevention.